Ensuring Coverage For American Indian and Alaska Native Children: An Assessment Of The Medicare Access and CHIP Reauthorization Act Outreach and Enrollment Round III Grantee Activities, July 2017–June 2018
Background
Children’s access to health insurance in the United States has improved dramatically over the past two decades. Driven largely by the availability of public health insurance provided through Medicaid and the Children’s Health Insurance Program (CHIP), the rate of uninsurance among children has dropped from about 15 percent in 1997 to 5 percent in 2017 (Bennefield 1998; U.S. Census Bureau 2018).
Despite this progress, as of 2017, nearly 4 million children were uninsured (U.S. Census Bureau 2018). In particular, more work is needed to find and enroll harder-to-reach populations, especially American Indian/Alaskan Native (AI/AN) children. Although they too have benefited from the expanded availability of public health coverage, 8 percent of AI/AN children were uninsured in 2016, nearly double the rate of uninsurance for all children in the United States that year (Haley et al. 2018). Better access to high-quality health insurance and health care could help address diabetes, chronic liver disease, heart disease, and other illnesses that are more common in AI/AN populations than other population groups in the United States (Center for Medicaid & CHIP Services 2016).
Connecting Kids to Coverage
To reach, enroll, and retain more children in Medicaid and CHIP, the Centers for Medicare & Medicaid Services (CMS) launched the Connecting Kids to Coverage (CKC) National Campaign and Grants Program in 2009. These initiatives have three primary goals:
- Raise awareness about Medicaid and CHIP
- Motivate parents to enroll their eligible children and teens and renew their coverage
- Provide free materials to help states, community groups, and others conduct successful outreach activities (InsureKidsNow.gov not dated)
Beginning in 2010, CMS launched a CKC grant program focused on enhancing outreach and enrollment support for AI/AN children. To date, CMS has awarded three rounds of Tribal outreach grants to AI/AN organizations and made available $10 million in the first round, $4 million in the second round, and $4 million in the third round (InsureKidsNow.gov 2017).
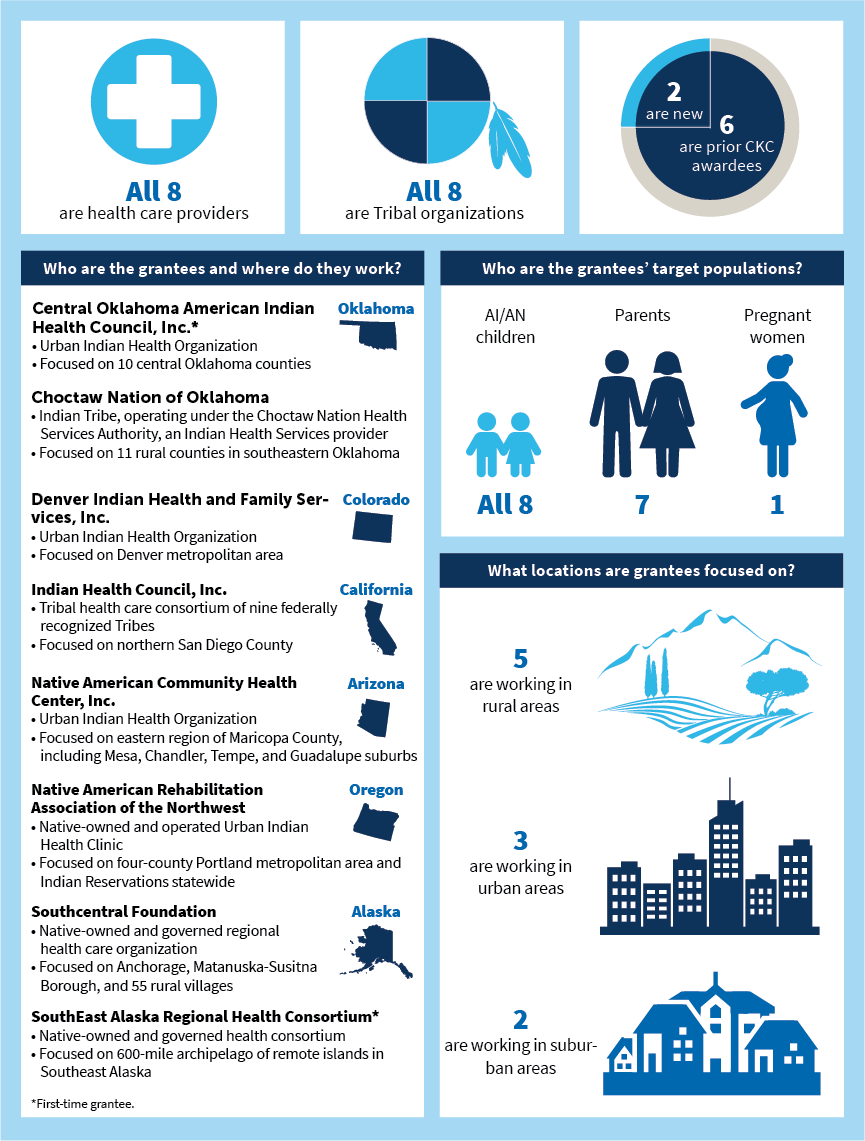
CMS contracted with Mathematica Policy Research to evaluate and report on grantees’ performance, and to provide technical assistance to help support grantees. This evaluation summary describes the first-year experiences of the eight Round III cooperative agreements with AI/AN organizations (Figure 1). It is based on a review of grantees’ progress reports covering the first year of their two-year grants, July 2017 through June 2018.
Key Findings
Outcomes
Many families benefited from grantees’ efforts during the first year of Round III grants:
- The eight Round III grantees serving six states supported application and renewal form submissions for more than 7,000 children, helping 6,029 children gain or renew Medicaid or CHIP coverage from July 2017 to June 2018. Across all eight grantees, renewals outpaced new enrollments, with 3,589 renewals compared to 2,440 new enrollments, although this varied at the grantee level. About 80 percent of the children grantees helped to newly enroll or renew coverage were of AI/AN descent (six of the eight grantees tracked this data).
- Five grantees—Central Oklahoma American Indian Health Council, Inc. (Central Oklahoma), Denver Indian Health and Family Services (Denver Indian Health), Native American Community Health Center (Native Health), Native American Rehabilitation Association of the Northwest (NARA-NW), and Southcentral Foundation (SCF)—have already achieved 40 percent or more of their two-year child enrollment and renewal targets. To date, two of the three grantees that have not met their targets serve exclusively rural areas, and one of these is also a new CKC grantee. Several factors might have contributed to the challenges faced by these grantees, however, conducting outreach in very remote rural areas sometimes prevented the grantees from being able to contact or follow up with prospective applicants. Some of the barriers experienced by grantees included limited or no roads, poor road conditions, bad weather, challenging geographic terrain, and little or no internet or phone access.
Figure 1. Characteristics of Round III grantees
Source: Mathematica’s analysis of grantees’ semiannual reports for the period July 1, 2017, to June 30, 2018, as well as grant application materials.
Activities
Round III grantees engaged in a number of activities to help AI/AN children and families enroll or renew coverage:
- All Round III grantees regularly engaged in one-on-one enrollment and renewal assistance and conducted outreach and education activities at their own clinics, at partner locations, and at community events.
- Round III grantees also staffed outreach, education, and enrollment booths at events they thought AI/AN families would be likely to attend, such as parent–teacher meeting nights at local schools, community festivals, and powwows.
- Grantees reported two strategies as most effective for increasing coverage. First, grantees said that forming partnerships with groups that have access to the target populations was an effective outreach strategy. Second, as Indian health care providers, many of the grantees used insurance coverage data to identify uninsured children or parents (or those nearing their renewal date), and then offering help to enroll or renew coverage.
- Grantees reported inconsistent experiences with school-based activities, and most grantees said attending community events did not lead to new enrollments or renewals.